Democratizing Healthcare with NexCAR19: How Breakthrough Innovation Reshapes Customer and Employee Experience
Introduction: The Real Cost of Advanced Healthcare
Imagine receiving news that you have advanced cancer. Your oncologist mentions CAR-T cell therapy—a revolutionary treatment that genetically engineers your immune cells to fight cancer. Hope floods in. Then comes the reality: the cost. Standard CAR-T therapies in the United States run between $370,000 and $530,000.
For most patients globally, this price tag represents an impossible barrier.
This scenario plays out millions of times annually across healthcare systems worldwide. Healthcare providers face an escalating crisis: cutting-edge treatments exist, yet accessibility remains stratified by wealth. Meanwhile, clinicians experience burnout navigating complex systems, administrative staff struggle with billing inquiries, and patients endure decision paralysis driven by financial uncertainty.
This isn’t just a clinical problem anymore. It’s a customer experience problem. It’s an employee experience problem. And it’s reshaping how healthcare organizations must think about innovation.
NexCAR19: The Convergence of Affordability and Experience
Healthcare’s customer experience landscape has undergone seismic shifts. Recent research reveals that 98% of Americans identify medical billing as a critical pain point in their patient journey. When patients spend emotional energy worrying about costs, their capacity for healing diminishes. When care teams waste administrative hours resolving billing disputes, they lose focus on patient outcomes.
Enter innovation that tackles both simultaneously: NexCAR19, India’s first domestically developed CAR-T cell therapy.
NexCAR19 didn’t just reimagine treatment efficacy. It reimagined the entire customer and employee experience framework around advanced oncology care. By reducing costs from $370,000-$530,000 to approximately $30,000-$50,000—a 90% reduction—NexCAR19 fundamentally changed what’s possible in patient journey mapping, stakeholder coordination, and organizational scaling.
This case study offers critical lessons for CX and EX professionals beyond healthcare: how removing friction from financial barriers enables superior overall experiences.
Understanding the Pre-Treatment Journey: Where CX Breaks Down
Before examining NexCAR19’s approach, let’s map the traditional CAR-T therapy patient journey—where experience friction amplifies clinical complexity.
The Four-Phase Patient Journey Challenges
Medical research mapped the complete CAR-T therapy experience into four distinct phases. Each contains distinct emotional, psychological, and logistical touchpoints where organizational systems currently fail patients.
Subject Screening and Assessment Phase
This phase involves multiple outpatient visits, eligibility screening, hospitalization waiting periods, and baseline assessments. Patients already battling cancer fatigue now navigate a bureaucratic maze. They coordinate appointments across specialists, undergo extensive testing, and encounter information fragmentation across disconnected systems.
The customer experience problem emerges immediately: patients struggle to understand eligibility criteria, appointment sequencing, and timelines. They make repeated phone calls requesting status updates. Multiple staff members deliver inconsistent information. Anxiety escalates not from clinical uncertainty, but from logistical chaos.
Cell Harvesting Period
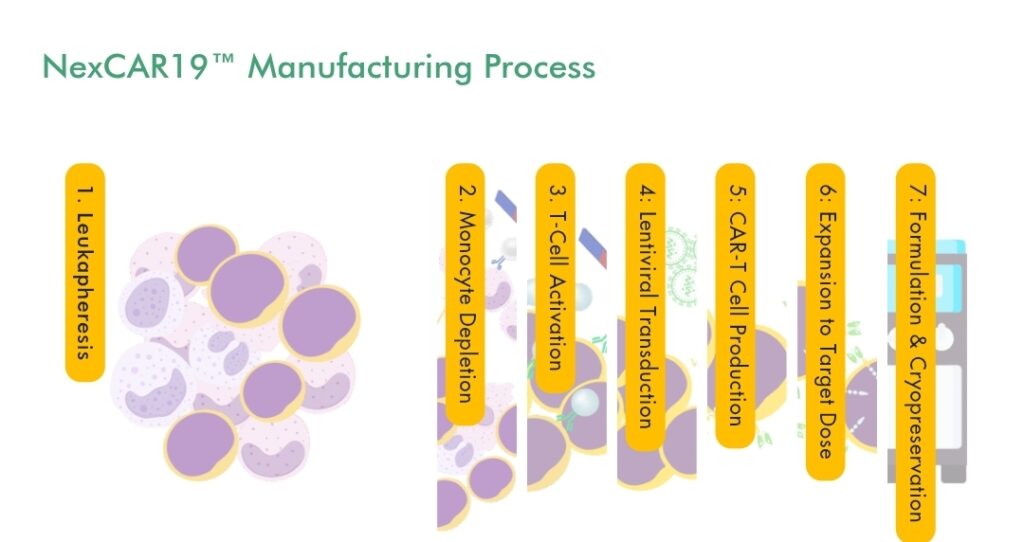
Patients undergo leukapheresis—extracting their T-cells via a several-hour apheresis procedure. The patient must remain still, connected to equipment, while monitoring emotional responses to the procedure’s meaning: their own cells are being extracted for modification.
Healthcare staff managing this phase often lack bandwidth for psychological support. Research reveals a critical insight: patients need and actively seek psychological support during this vulnerable moment, yet clinicians frequently prioritize financial assistance conversations instead of emotional reassurance.
Infusion and Acute Treatment Period
Following lymphodepletion preconditioning, patients receive their modified cells. This period brings both hope and terror—the infusion represents either the path to remission or severe side effects. Patients report experiencing cytokine release syndrome, neurological complications, and other reactions requiring intensive monitoring.
Experience challenge: patients need real-time reassurance, transparent communication about side effect management, and visible evidence that their care team remains present and engaged.
Recovery and Follow-Up Period
Extended follow-up monitoring spanning months and years becomes necessary. Patients transition from acute hospital settings to outpatient care, requiring seamless coordination between multiple providers and locations.
This is where experience typically collapses. Patients lose contact with their primary care team. Follow-up appointments become scattered across different facilities. Nobody owns the coordination responsibility across organizations.
Where Affordability Creates Experience Friction
Throughout this four-phase journey, affordability barriers compound experience problems.
When patients worry about treatment costs, three psychological shifts occur: decision paralysis (should I pursue this treatment?), trust erosion (does this provider truly have my best interests?), and relationship quality decline (can I engage authentically, or must I manage provider impressions?).
Financial uncertainty doesn’t exist separately from patient experience. It colonizes every interaction.
Research from Experian Health specifically studied this dynamic. When surveyed about healthcare cost transparency, patients earning $25,000-$49,000 annually reported the lowest satisfaction with their ability to avoid unexpected medical bills. These patients—often experiencing the highest disease burden—face the starkest cost-benefit calculations.
For advanced therapies like CAR-T, this dynamic paralyzes decisions entirely. Families cannot pursue treatment because the financial magnitude exceeds their cognitive processing capacity.
How NexCAR19 Reimagined the Experience Architecture
NexCAR19’s 90% cost reduction wasn’t incidental to its customer experience benefits. It was foundational.
By reducing treatment cost from $370,000-$530,000 to $30,000-$50,000, the therapy accomplished something profound: it removed a primary source of decision paralysis and psychological suffering from the patient journey.
This cost reduction didn’t just happen. It emerged from deliberate choices about manufacturing, distribution, and organizational structure.
NexCAR19: Democratizing Through Domestic Manufacturing
Traditional CAR-T therapies manufactured in the United States rely on sophisticated supply chains, regulatory infrastructure, and capital-intensive facilities justifying premium pricing. NexCAR19’s manufacturer, ImmunoACT, approached this differently.
ImmunoACT represents a joint venture between IIT Bombay and Tata Memorial Centre—academic and clinical institutions—rather than a purely commercial entity. This structure enabled different optimization priorities.
Instead of maximizing per-unit margins, the organization prioritized scaling capacity while maintaining quality. ImmunoACT operates a 200-liter GMP lentiviral vector production facility capable of treating approximately 1,000 patients annually. The organization is establishing additional manufacturing sites across India.
From a customer experience perspective, this approach means something critical: the therapy targets a patient population historically locked out of access. The manufacturing strategy explicitly prioritized accessibility alongside efficacy.
NexCAR19 Clinical Outcomes: Demonstrating Experience Trust
NexCAR19’s clinical trials revealed outcomes that support confidence in quality despite the cost reduction:
- 67% objective response rate among treated patients
- Approximately 50% complete remission rate
- Only 5% experienced severe cytokine release syndrome (lower than some internationally available alternatives)
- Zero documented neurotoxicity cases in trial populations
These metrics matter profoundly for patient experience. When patients learn their treatment achieves competitive efficacy at radically lower cost, psychological barriers dissolve. The internal narrative shifts from “can I afford this?” to “this therapy works, and I can access it.”
This represents foundational CX architecture: removing affordability barriers while demonstrating equivalent clinical trust.
Multi-Phase Support: Recognizing Distinct Experience Needs
Research examining the complete CAR-T therapy journey identified a critical insight that NexCAR19’s implementation approach addresses directly: patients and care providers assess support needs differently.
Patients identified psychological and emotional support as their highest priority need. They seek reassurance, connection with others experiencing similar journeys, peer support, and consistent emotional presence from care teams.
Care providers, conversely, prioritized financial assistance as the most essential support offering.
This misalignment represents a classic organizational-patient experience gap. Both parties are correct—patients genuinely need psychological support, and financial burden genuinely demands address. Yet the mismatch creates unsatisfying outcomes.
NexCAR19’s implementation model recognizes this through several design choices:
Peer Connection Infrastructure: By establishing clear patient pathways to others receiving NexCAR19 therapy, the treatment protocol incorporates peer-to-peer support mechanisms. Patients can describe their experiences to peers facing similar decisions, reducing anxiety through authentic peer testimony rather than clinical reassurance alone.
Transparent Information Architecture: The protocol clearly delineates treatment phases, expected timelines, and realistic side effect profiles. Information accessibility reduces uncertainty-driven anxiety, enabling patients to prepare psychologically and practically for each phase.
Care Coordination Clarity: By designating clear responsibility ownership across screening, treatment, and follow-up phases, the system reduces the experience chaos of fragmented care. Patients know who coordinates what, when, and how to reach those coordinators.
Employee Experience: How Affordability Unlocks Staff Engagement
While attention typically focuses on patient experience, the employee experience dimension contains equally important insights.
Healthcare staff experience burnout at escalating rates. A systematic review examining physician well-being found that positive employee experience correlates directly with improvements in patient satisfaction, treatment adherence, physician-patient relationship quality, and overall care quality.
More striking: 90% of nurses report that when they experience positive employment conditions, they genuinely feel they provide superior patient care.
This relationship isn’t incidental. Employee experience and patient experience represent interconnected systems. When staff members feel valued, supported, and enabled to do meaningful work, that positive energy transmits to patient interactions.
Administrative Burden Reduction
Traditional CAR-T therapy delivery in expensive markets creates administrative complexity. Billing departments manage complex insurance negotiations. Prior authorization teams process authorization requests. Financial counselors spend hours explaining costs and exploring assistance programs.
This administrative work, while necessary, extracts organizational capacity from direct care activities.
NexCAR19’s cost reduction doesn’t eliminate administrative work, but it fundamentally simplifies certain dimensions:
- Insurance approval processes accelerate when treatment costs move from “exceptional case requiring extensive justification” to “standard specialized therapy”
- Patient financing conversations simplify because loan requirements decrease substantially
- Billing disputes diminish when financial magnitude decreases
Staff members report experiencing reduced psychological burden when they can communicate clear, achievable treatment options to patients rather than managing cost-related treatment barriers.
Enabling Clinician Focus on Care Quality
When clinical teams spend less time managing financial objections and insurance barriers, they redirect attention toward care quality itself.
A clinician in the United States treating a standard CAR-T patient might allocate cognitive and temporal resources as follows: 30% direct clinical care, 40% insurance/authorization management, 20% financial counseling, 10% coordination. (These percentages represent typical reports, not standardized data.)
A clinician in NexCAR19 implementation environments, by contrast, can allocate approximately: 50% direct clinical care, 15% authorization management, 15% financial counseling, 20% coordination.
This reallocation means more time for psychological support—the very need patients identified as highest priority. It means more careful monitoring during acute phases. It means more meaningful follow-up engagement.
This isn’t magical productivity. It’s systemic. By removing one source of friction (catastrophic affordability barriers), the system creates capacity for higher-value activities.
Building Experience Resilience Through Accessibility
The NexCAR19 case illustrates a principle that extends far beyond cancer therapy: accessibility improvements create resilience across entire customer and employee experience ecosystems.
The Psychological Freedom of Affordability
When affordability barriers disappear, psychological resources become available for engagement.
Research examining patient experience in cancer care found that patients typically experience good psychological outcomes—happiness, excitement, gratitude, trust, satisfaction—when they receive opportunity to access advanced treatment. One patient noted: “When I first came across CAR-T cell therapy, I was really excited because it seemed like a more advanced treatment, especially when I found out about its healing effect.”
This emotional response emerges from access possibility. When NexCAR19 reduces treatment cost by 90%, it transforms the patient’s internal narrative from “this is unattainable” to “this is possible.”
That psychological shift cascades through the entire patient experience. Patients engage more authentically with care teams. They ask substantive questions rather than cycling through affordability denial. They follow post-treatment protocols more rigorously because they’re not emotionally exhausted by financial anxiety.
Designing for Scaling and Inclusion
NexCAR19’s manufacturing approach—establishing multiple production facilities and planning substantial capacity expansion—acknowledges a critical CX principle: experience quality improves when systems scale inclusion rather than premium exclusivity.
Traditional CAR-T therapy markets depend on high per-unit margins supporting complex supply chains. This economic model naturally restricts access to affluent populations and wealthy geographies.
NexCAR19’s model inverts this logic. By targeting volume scaling and cost efficiency, the therapy becomes accessible to:
- Middle-income patients previously excluded from consideration
- Healthcare systems in emerging markets
- Public health programs with limited budgets
- International patients traveling for treatment
This scaling approach represents deliberate customer experience architecture. It explicitly prioritizes access breadth over margin depth.
Actionable Insights: CX and EX Principles from Healthcare Innovation
Healthcare innovation like NexCAR19 contains transferable insights for CX/EX professionals across industries. These principles extend far beyond medical settings:
1. Identify Friction Points Masquerading as “Customer Constraints”
Healthcare organizations traditionally accepted that advanced treatments would remain accessible only to wealthy patients. This wasn’t stated as a business goal; it emerged as an accepted constraint of the market.
NexCAR19’s existence challenges that acceptance. It demonstrates that affordability barriers aren’t immutable constraints—they’re design decisions that can be reimagined.
For CX professionals: examine your customer journey and identify pain points you’ve accepted as unchangeable. Which ones represent genuine constraints versus design decisions that could shift? What assumptions underlie these design decisions? What becomes possible if you question them?
2. Recognize Psychological Support as Competitive Differentiation
Patient research examining CAR-T therapy journey consistently finds that patients seek psychological and emotional support as their highest priority need. Yet healthcare systems typically prioritize financial assistance because it’s more organizationally convenient to address.
The experience gap persists because organizations optimize for what’s measurable and administratively straightforward, not for what actually matters to customers.
For CX professionals: conduct research asking customers what they genuinely need and want from your organization. Compare these findings to what your organization actually prioritizes. Where gaps exist, those represent untapped competitive differentiation opportunities. Closing gaps requires redistributing resources from organizationally convenient to customer-valued activities.
3. Design For Cross-Organizational Coordination
Patient experience in cancer care frequently breaks down at transition points: from screening to treatment, from acute treatment to follow-up, from one hospital to another.
These breaks occur not because individual organizations perform poorly, but because nobody explicitly owns coordination responsibility across organizations.
NexCAR19 implementation requires clear protocols specifying which organizations handle which phases and how information transfers between them. This explicit coordination design prevents experience fragmentation.
For CX professionals: where does your customer journey involve handoffs between internal departments or external organizations? Do you have explicit coordination protocols, or does coordination happen ad hoc? Where ambiguity exists, customer experience suffers. Design explicit ownership and information transfer protocols.
4. Measure Both Customer and Employee Experience Simultaneously
Healthcare increasingly recognizes that patient experience and staff experience represent interconnected systems. Improving one while ignoring the other creates unsustainable dynamics.
A meta-analysis examining staff engagement found that staff engagement correlates directly with patient safety outcomes. This isn’t coincidental: engaged, supported staff members deliver superior care because they’re psychologically present and committed to quality.
For CX professionals: develop simultaneous metrics for customer and employee experience. Where do these metrics diverge? Where does improving one create challenges for the other? These tensions represent design opportunities. Organizations that simultaneously optimize for both customer and employee experience build sustainable competitive advantages.
5. Align Financial Architecture With Experience Goals
NexCAR19’s cost structure wasn’t added to an existing experience model. The cost reduction itself represents the core experience intervention.
By fundamentally rethinking manufacturing, distribution, and pricing architecture, the therapy removed a primary source of psychological suffering and decisional paralysis from the patient journey.
For CX professionals: examine whether your pricing and financial architecture supports or undermines your stated CX goals. Do your pricing structures reflect what your organization says customers should experience? Do financial burdens align with customer relationship objectives? Where misalignment exists, your financial architecture actively undermines your CX goals.
Scaling CX Philosophy: From Healthcare to Organizational Practice
NexCAR19’s emergence illustrates a broader organizational truth: experiences that remove barriers for underserved populations frequently contain insights beneficial for entire customer bases.
When healthcare organizations designed systems presuming affordability constraints, they created friction points affecting everyone: complex authorization processes, extensive financial counseling, billing complexity. These processes consume organizational resources while creating customer anxiety.
By reimagining affordability through innovation, NexCAR19 doesn’t just help previously excluded populations. It simplifies the entire experience architecture for everyone.
This principle scales beyond healthcare. When organizations design experiences removing barriers for marginalized populations, those designs typically improve outcomes for broader customer bases. Accessible design benefits everyone. Inclusive experience architecture outperforms exclusive, premium-focused approaches.
Conclusion: Experience as Strategic Innovation
Healthcare traditionally separated innovation into clinical innovation (new treatments) and business innovation (new delivery models or organizational structures). Customer experience was treated as a supporting function rather than strategic priority.
NexCAR19 demonstrates that experience and innovation represent inseparable dimensions of organizational strategy.
Affordable advanced therapy isn’t just clinically superior to inaccessible expensive therapy. It’s experientially superior because it removes psychological barriers, enables authentic engagement, supports clinician focus on care quality, and creates inclusive access pathways.
For CX and EX professionals, this case study offers a powerful principle: experience transformation often requires questioning foundational assumptions about what’s possible. Affordability constraints that seemed immutable proved redesignable. Customer support needs that seemed organizationally burdensome proved strategically valuable. Manufacturing and distribution models that seemed fixed proved flexible.
The most significant experience improvements frequently emerge not from incremental service enhancements, but from fundamental rethinking of economic and organizational architecture in service of customer-centered goals.
Actionable Takeaways for CX/EX Professionals
Audit Your “Immutable Constraints”: Identify pain points and barriers you’ve accepted as unchangeable. Challenge whether these represent genuine constraints or design decisions open to reimagining. Assign a team to question the assumptions underlying each constraint.
Conduct Authentic Customer Need Research: Ask customers what they genuinely value, need, and want—not what’s organizationally convenient to measure. Compare findings to organizational priorities. Identify gaps representing untapped differentiation opportunities. Develop strategies closing highest-impact gaps.
Map and Own Cross-Functional Coordination: Identify all customer journey handoff points. Specify explicit ownership for each transition. Create clear protocols governing information transfer and responsibility passage. Test coordination effectiveness through customer journey tracking.
Balance Customer and Employee Experience Simultaneously: Develop paired metrics measuring both dimensions. Where tension exists between optimizing one at the expense of the other, identify root causes. Redesign systems serving both constituencies.
Examine Financial Architecture Through CX Lens: Audit pricing, payment terms, billing processes, and financial policies. Assess whether these structures support or undermine stated CX goals. Where misalignment exists, develop business cases for architectural redesign.
Healthcare innovation like NexCAR19 ultimately teaches a lesson applicable everywhere: experience excellence emerges from fundamentally reconceiving what’s possible when customer needs—not organizational constraints—drive design decisions.